|
| Source: my back garden |
Really,
the majority of us are somewhere between normal and dysfunctional. Most of
us can improve our breathing and feel many potential benefits from doing
so. These benefits can be better sports performance, improved
mobility in the spine and rib-cage, improved core strength (as the
diaphragm is a key part of our core (see Getting down to the Core blog)), less
pain in neck and shoulder muscles and also decreased stress levels.
I would call this normal breathing optimal breathing as we can work towards it and for many of us it isn't yet normal!
Optimal breathing uses the diaphragm for 75% of effort and the intercostals between the ribs account for the remaining 25%. This means that neck and shoulder muscles are barely used to breathe with.
 |
| Source: Wikimedia Commons |
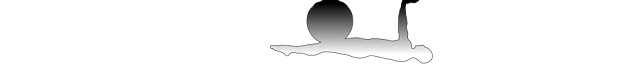
The diagram above shows, as we inhale, the diaphragm contracts and it's outer edges pull the ribs outward and upward. The intercostal muscles help by pulling the ribs further apart. The thoracic cavity expands and air is drawn into the lungs.
At the same time, the abdominal cavity is compressed and the abdominal and pelvic organs move down meaning the abdominal wall has to expand outwards and forwards to accommodate this. The transverse abdominus relaxes and the pelvic floor descends as it receives the increased load of abdominal and pelvic organs.
In the optimal exhale the diaphragm elastically recoils back up higher into the rib cage, abs and pelvic floor contract and the intercostals relax. This sends air back out of the lungs.
It
sounds simple, so why don't we all breathe optimally? Well chances are
that we did when we were young. And then something changed and our
breathing changed too. This might have been a physical change to our
body - such as our spine and rib-cage stiffened with a lifestyle of
sitting and inactivity or we may have had a baby which can both change
our spinal alignment and the position of the diaphragm. Or it might be that stress and anxiety have changed the
optimal breathing to something more rapid and shallow.
The
most common breathing dysfunction is chest breathing (referred to as
'thoracic' breathing in the paper). This type of breathing is short
exhalation followed by shallow inhalation. Muscles in the neck and
shoulders overwork to sustain this. The position of the ribs may well
be altered so the front, lower ribs flare upwards. There is likely to
be a lack of mobility in the lower ribs and potentially muscle pain in
the neck and shoulders.
So, where to start on
retraining your breath? In many cases it's about re-acclimatising the
brain to higher CO2 levels by gradually using longer exhales. And
breathing into the back and the sides of the rib-cage, activating the diaphragm more to encourage fuller inhalation.
The paper concludes that "future research is needed to validate breathing re‐education programs
and the role they have in treating pain disorders, preventing injury,
and improving movement patterns." Joseph Pilates understood this many years ago - so perhaps your first call when looking to improve your breathing technique should be your Pilates teacher...
Many thanks to Heather King-Smith for her fantastic Breathing and Alignment training.
* Bradley H & Esformes J Breathing Pattern Disorders and functional movement. Int J Sports Phys Ther. 2014 Feb; 9(1): 28–39.